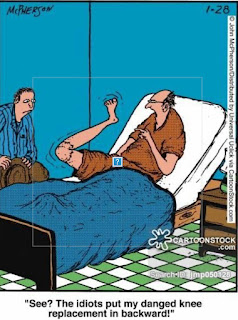
The truth about total knee replacement....
Or: the rest of February! And March! And April!!!
Nothing had prepared either of us for the
level of pain I experienced post-op.
The pre-op assessments had all seemed
comprehensive and straightforward: blood tests, ECG, explanations from
physiotherapists, even occupational therapists (which seemed to be mainly about
how to put one’s underwear on). There were all kinds of leaflets to read about
what to expect, what the spinal anaesthetic procedure would be, and so on. I felt
well-prepared and excited to be finally ‘fixing’ the arthritic knee which has
limited my activities for over the last dozen years.
Going into hospital – after the op had been
delayed by three weeks – was easy. My operation was scheduled during ‘Closure
Week’ when, normally, there wouldn’t be many operations going on. So,
initially, there were just two of us on a nine-patient ward and I was fortunate
to have a room and bathroom to myself. The staff were all very friendly, the
anaesthetist – who I hadn’t met previously – was kind and competent, sedating
me after the spinal so that I drifted off after just a couple of minutes in the
anaesthetics room, only coming gently round as I was wheeled out of theatre.
Such a pleasant experience compared with the general anaesthetics I had had
more than 35 years previously.
Back at the ward, I was given painkillers
for when the ‘spinal wore off’, and then the ‘fun’ started. More pain in my leg
than I had ever experienced, including appendicitis and the worst of
toothaches, which seemed to consume my whole body. Agony.
Eventually, midway through the night (I had
been returned to the ward at around 5pm, still blissfully unaware and able to
drink a cup of tea with a delicious egg sandwich), my whimpering caused the
staff to take pity on me, giving me morphine and more tea and toast. I was,
initially, able to drift off for half an hour for a short nap but was soon then
awake.
That night, and subsequent nights, seemed
to last forever. Morphine had little effect: otherwise I was only given a
normal dose of intravenous paracetamol, eventually moving on to paracetamol
tablets and codeine tablets in preparation for discharge.
Physio began almost immediately. One lovely
nurse – Karenjoi – warned me that the physio could be a bit ‘aggressive’ and
dosed me up with painkillers in good time beforehand. Welcome relief,
afterwards, was a bag of ice on my injured knee.
She wasn’t kidding. Every move I made felt
as if the stitches – 20 cm of them – were tearing open as pain ripped down my
knee and shin. My muscles barely seemed to work: I could only move my operated
leg on and off the bed by rotating my whole body and supporting the leg with
the ankle of my good leg: a useful tip from the physios. To start with, my leg
completely refused to bend, remaining stubbornly stuck straight out in front of
me. Nevertheless, I practiced the exercises as best I could, transferred myself
from a walker onto crutches (still looking like a ninety year old granny – I
have the photo to prove it), ‘walked’ along the corridor and then up and down
the stairs – and was then signed off as fit to leave the hospital.
Still, once home I found I could manage the
bathroom well with first 2 crutches, then 1, holding onto the washbasin to
lower or pull myself up. By 3 weeks, I
was almost walking unaided.
There was a steep learning curve in the
interim.
I found myself phoning the nurses at the
Medical Specialist Group a couple of times. My foot and ankle has swelled up
hugely: is that normal? (Yes.). Are these levels of pain normal?
(Disappointingly, yes. Keep taking the paracetamol and codeine.) And, embarrassingly:
I double dosed on paracetamol by mistake: does it matter? (No – there were 3
hours between the two doses, so not too awful.) I was grateful for the calm,
friendly voice at the other end of the phone line.
I discovered that icing under the knee,
using a sandwich of 3 freezer ice packs rather than a bag of ice (which had a
tendency to leak!), was as useful as icing on top of it.
Waking in the night from pain – which I did
frequently – meant that I needed to move, whether a short walk around the house
to relieve the cramping muscles, or a change to a comfortable recliner chair.
The pain was considerably worse at night,
as the body used the night hours to focus on healing. I became so stiff that
the pain woke me: putting headphones in and listening to David Suchet read the
psalms, via BibleGateway, was a soothing distraction.
After a week or so, I stopped taking
codeine during the day, tried, at first, to reduce it at night but then went
back up to a normal dose until I felt I could reduce it again.
A heat pad on the back was invaluable,
soothing knotted muscles and aching bones.
And friends came, and came… such a
blessing. They brought meals, flowers, chocolates – but most of all, they
brought love and care and a welcome distraction from all the pain. The days
when there were no 6 Nations Rugby matches and no visitors (sometimes I’d had
three lots in a day, so I wasn’t complaining!) seemed endlessly long. I read,
played puzzles, coloured the lovely prayer journal which Adele had ordered for
me; messaged on WhatsApp to friends and family far away; and read far too much
on facebook, scrolling to distract myself.
One particularly useful diversion, which
took my mind off the inevitable pain and discomfort when doing the exercises,
was to watch the BBC game show Would I Lie To You? Fun. I tried one or two other recommendations, but
that was definitely the most effective.
By 3 weeks, days were enjoyable – if slow
when no one dropped in to visit – but the nights still trial. I was signed off
work for 12 weeks total: still a way to go, so practicing patience was in
order.
One delightful addendum: my op was
scheduled for February 14th: Valentine’s Day. We don’t usually
‘celebrate’ it, but this time, Richard sent me a delightful set of emojis: 👩❤👨
🐈⬛ 🕰 ❤ I had to have it explained to me: 2people+
heart, is us then dog all waiting for their loved
one to come back. Never mind that the ‘dog’ was a cat! So sweet
of him. He has been absolutely fantastic: so thoughtful and attentive,
uncomplainingly fetching and carrying for me, cooking breakfast and other
meals, driving me to appointments…
The second half of February, then,
passed by in a blur of pain. My stitches were removed by a nurse at MSG at the
end of the month: a fascinating picture. It all looked much neater and cleaner
than I was expecting: indeed, at my pre-op check the nurse had sighed, “Oh, Mr
Hopcroft does the neatest scars,” and that was certainly the case.
I was still using two crutches when I
had my first physio appointment two weeks after the operation, but soon
graduated to one and then, four weeks after, I could just about walk without any
at all, just using a stick occasionally.
The physio, Peter, was brilliant. He
answered my many questions very patiently.
What position should my knee be in? Straight.
(Not what I wanted to hear – that was quite uncomfortable.) Can my leg lean to
one side? No, it should be straight. (Again, that was uncomfortable.) How painful should it be to do the exercises?
As painful as you can bear it.
I had, in fact, mostly picked that up
from the internet – which was not hugely helpful until I discovered the website
of the Royal Orthopaedic Hospital in Birmingham which proved to be a mine of
commonsense and practical advice. Still,
it was good to get it confirmed.
He was very kind, but there really wasn’t
much either of us could do about the pain, although I did have some
leg-stretching exercises I could do when the pain woke me up.
Which it did, frequently. My sleeping
pattern was awful for over seven weeks. I would, perhaps, sleep for the first
two hours before the pain in my leg muscles woke me up. Then, if I was lucky, I
would doze, woken by pain at hourly intervals. Sometimes it was my outer calf
muscles, then behind the knee, or sometimes the lower thigh. Referred pain
caused discomfort in my lower back and top of the thigh/groin area. A warm wheatbag
helped enormously, though in my zeal to heat it up, I managed to set fire to it
a couple of times when warming it up in the microwave, resulting in a wonderful
smell of burnt toast, several wheat grains scattered among the sheets and
several sessions of repairs involving needle and thread.
I found myself awake every night.
Getting up and walking around helped the pain initially, loosening up the
muscles, but then I could not settle. I would go into the sitting room, where a
reclining chair and mattress, complete with blankets, cushions and duvet, would
be waiting. If I was lucky, I would doze off at around 4 or 5 am for an hour or
so…
But, of course, I could catch up during
the day. Naps lasted from an hour to a full morning or afternoon, but I didn’t
fret, reasoning that my body would sort itself out eventually once the pain
became more manageable. I had been sent out from hospital with a long prescription
for paracetamol and codeine – two weeks’ worth. By the end of one week of
taking this – not even two weeks after the operation – I realized that the pain
was not going to go away quickly, so I started reducing the codeine during the
day so that I could stretch the period during which I would take it, keeping it
for the night hours. And, although there were no directions to do so, I slowly
reduced the daily dose until, from an initial 240mg a day, I was taking only
30mg.
Wow. A good thing too. Coming off the
codeine was very unpleasant. I felt quite unwell for the first two weeks
without it, feeling as if I had stomach flu, and it wasn’t until the end of the
third week that I felt I was getting back to normal. Never again. I wasn’t even
sure that it was particularly effective.
I persevered – as I had been encouraged
to do by every knee replacement patient I had spoken to – with the exercises.
Three times a day, varying with each physio visit, and sometimes so painful that
I felt sick and dizzy, yet by 8 weeks after the op my knee had reached a
wonderful 120 degrees of flexion and I was almost pain-free. So much so, that Peter
then discharged me with the proviso that I could return within a couple of
months if I needed to. Meanwhile, it was ‘business as usual’ – returning to
gentle arms-only with perhaps front crawl legs swimming, careful and limited cycling
and continuing on with the exercises to improve strength and maximise the gains
made. Wonderful. And, even better, I was sleeping until around 5 am. I diligently
massaged the scar with cream and lavender oil, watching it slowly fade with
satisfaction.
Back to gardening, too, though found
that very tiring to start with.
Still, by mid-April I was well on the
mend… and still another month to go before I had to return to work…
Two months of pain, discomfort and
weariness. But friends had been marvellous, visiting so much especially during
the first month, bringing ready meals of all kinds – even Korean! – chocolate,
baked goods and flowers. So very, very kind. It was great to be able to sit and
chat, and of course I had a lot of time for reading, too. Slowly, my brain
began to return to normal…